Abstract
Introduction
Rosai-Dorfman disease (RDD) is a rare subtype of non-Langerhans cell histiocytosis that is classically characterized by lymphadenopathy and accumulation of CD68-positive, S100-positive, and CD1a-negative histiocytes with frequent emperipolesis in sinuses of lymph nodes and lymphatics of internal organs. In this series, we report on the clinical features, treatment strategies utilized and outcomes of a large cohort of RDD patients seen at one institution.
Methods
We retrospectively reviewed the medical records of patients with biopsy-proven RDD evaluated at the Mayo Clinic from January 1, 1994 to September 2, 2016. Data abstracted from the medical records included: demographic characteristics, symptoms at disease presentation, treatment, and outcomes. In addition, radiologic and molecular findings were collected when available.
Results
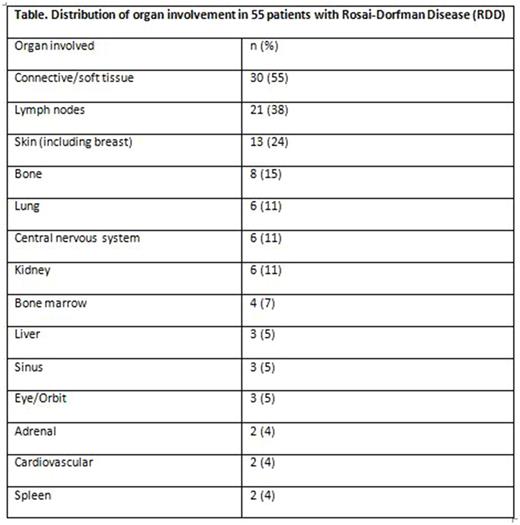
A total of 55 patients with confirmed RDD were included in our study. The median age at diagnosis was 50 years (range, 2-79), including 4 pediatric subjects. The median duration from symptom onset to diagnosis was 6.4 months (range, 0-128; mean 18 months). There was a female preponderance (male 1: female 1.5). The most common presenting signs and symptoms were painful or painless subcutaneous masses (40%), lymphadenopathy (13%), bone pain (11%), constitutional symptoms (fevers, chills, myalgia, or weight loss: 11%), and abdominal pain (11%). The organ systems involved with RDD based on either histopathological or radiological findings are shown in the Table. In our series, extranodal presentation in the soft tissue (55%) was more common than a nodal presentation (38%). Other rare extranodal sites included one case each involving the parotid gland, thyroid gland, testicles, and rectum. The median number of biopsies required to establish diagnosis was 2 (range, 1-6). Next generation sequencing was performed on 2 patient samples, and showed a CDC73 truncation in exon 5 in the first case and a KRAS K117N mutation in the second case. BRAF V600E mutation testing was negative in 2 patients: one by immunohistochemistry and one by urine cell-free DNA PCR.
Treatment data were available for 46 patients. Of these, 13% patients were observed. The most common first line therapeutic modalities used were surgical excision (39%) and corticosteroids (35%). Other first-line systemic therapies included rituximab in 2 patients and vinblastine in 1 patient. Approximately 13 (28%) patients developed recurrent disease and were treated with other modalities: surgery (n=4), radiation therapy (n=3), and systemic therapies like cladribine (n=4), CVP (cyclophosphamide, vincristine, and prednisone; n=1), and 6-mercaptopurine with prednisone (n=1).
The median duration of follow-up after diagnosis was 20 months (range, 0-188). At the time of last follow-up, 4 patients were deceased. Of the deceased, 3 patients died from other malignancies (acute myeloid leukemia, peripheral T-cell lymphoma, and metastatic gall bladder carcinoma) and the cause of death for 1 patient was unknown.
Conclusions
RDD is a rare histiocytic disorder presenting with diverse clinical manifestations. The diagnosis is often delayed due to inconclusive biopsies, and in some instances, multiple biopsy attempts are necessary to secure a definitive diagnosis. Approximately one-third of patients may require second-line systemic therapies. Next generation sequencing might yield targetable mutations in RDD patients that relapse or have progressive multi-organ disease.
Nowakowski: Morphosys: Consultancy, Research Funding; celgene: Consultancy, Research Funding; Genetech: Consultancy, Research Funding; Bayer: Consultancy, Research Funding; pharmacyclics: Consultancy; Abbvie: Consultancy; Nanostring: Research Funding. Sher: LAM Therapeutics, Inc: Research Funding. Parikh: Pharmacyclics: Honoraria; Pharmacyclics: Research Funding; AstraZeneca: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal